A recent review, authored by researchers at Monash University, Australia, looks at potential sources of IgE and suggests how these could serve as therapeutic targets for allergic diseases. We share some of their observations here, including the importance of mouse models to advance understanding of IgE biology, and comment on how Jackson ImmunoResearch Anti-Human IgE Antibodies can help to reveal novel discoveries.
Sensitization is a critical factor in the development of allergic diseases
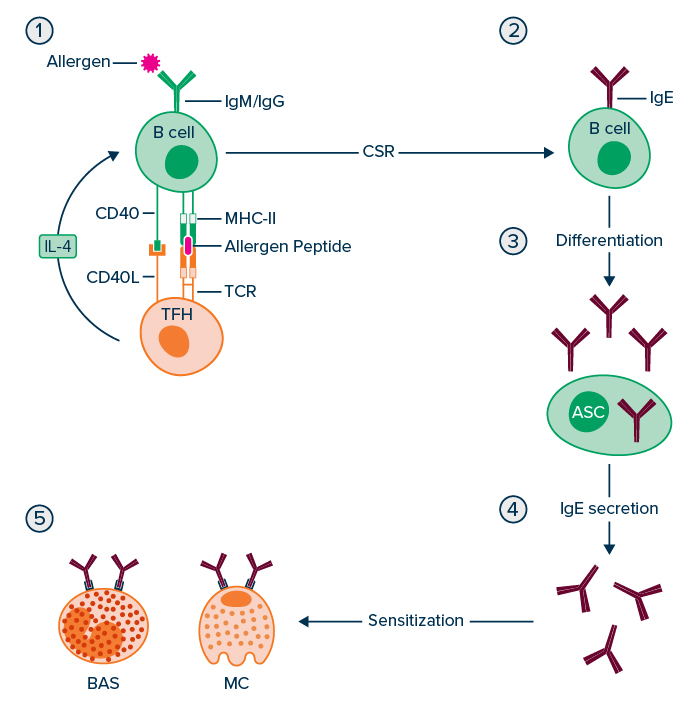
While IgE is the rarest secreted antibody isotype, it represents a key mediator of allergy and associated diseases such as asthma and eosinophilic esophagitis (an allergic inflammation of the esophagus that typically occurs in response to certain foods). Sensitization, summarized in Figure 1, is a critical factor in the development of such conditions that involves the maturation of B cells into IgE antibody-secreting cells (IgE+ ASC) and subsequent binding of IgE to receptors on the surface of mast cells and basophils. Notably, sensitization paves the way for allergen re-exposure to trigger an allergic response, which can vary in severity from mild tissue edema to fatal anaphylaxis.
Sensitization is difficult to reverse
Over the past few decades, various attempts have been made to limit the impact of sensitization and thus reduce the severity of disease. However, efforts have been hampered by gaps in researchers’ understanding of IgE biology, which include how long IgE+ ASC persist, and which B cells are responsible for ongoing IgE+ ASC production in non-remitting allergies. Despite this, encouraging results include the finding that the Bruton’s tyrosine kinase (BTK) inhibitor remibrutinib inhibits activation of human basophils and mast cells induced in vitro and the discovery that monoclonal antibodies targeting IgE can alleviate allergic symptoms.
Allergen type and exposure method can impact sensitization
It is now known that allergens differ in terms of how likely they are to sensitize, whether they will elicit their effects throughout an individual’s lifetime, and if they will co-sensitize to other allergens. For example, milk and egg allergies usually predominate in infants and resolve by age 12, while allergies to peanuts, fish, and shellfish tend to persist, and cockroach-allergic individuals are often co-sensitized to house dust mites. In addition, the manner in which an allergen is first encountered can impact sensitization. Common routes of sensitization include chronic respiratory exposure to environmental allergens, exposure to food proteins (typically during the first three years of life), and exposure resulting from skin damage.
Mouse models of allergy reflect different sensitization routes
Mouse models of allergy have been widely used to study the mechanisms of IgE production and are designed to reflect the sensitization routes just described. They include models based on long-term exposure to aerosolized allergens, which mimic chronic workplace exposures by maintaining a low-level IgE response for extended periods of time, and models involving adjuvanted mucosal exposure through the gut or lung, which have utility for investigating the auto-adjuvant properties of allergens such as papain and Der p 1. Models based on tape-strip damaged skin allow for studying allergen exposure through skin lesions, including those associated with eczema and filaggrin loss-of-function mutations.
IgE+ ASC demand further investigation
Although sensitization is known to result in the production of IgE+ ASC, there is still much to learn about these cells. For example, while IgE+ ASC have been suggested to come from a germinal center (GC) or post-GC memory B cell (mBC) source, this remains unclear. Although mouse work indicates that IgG B cells are the main reservoir of IgE+ ASC precursors in the context of allergen re-exposure, two recent studies infer that a subset of memory B cells might harbor IgE memory in humans. The lifespan of IgE+ ASC is also highly contentious. Although transcriptomic evidence has confirmed the existence of immature IgE+ ASC, the presence of long-lived IgE+ ASC has yet to be verified. A further area for investigation involves determining whether blocking the IL-4 signaling required for IgE CSR could provide therapeutic benefit. Encouraging clinical results have been seen using the anti-IL-4Rα antibody dupilumab for this purpose, including >80% loss of serum IgE over treatment periods of 1 year or more in allergic asthma, allergic rhinitis, and atopic dermatitis patients. Answering these questions, and others, is essential to develop effective treatments for IgE-mediated diseases.
Supporting allergy research
When studying the role of different immunoglobulin isotypes in a biological mechanism, it is important that they are detected specifically to prevent misidentification and illuminate the role of each isotype in the process. Jackson ImmunoResearch specializes in producing secondary antibodies for life science applications and offers Anti-Human antibodies specific to IgG, IgA, IgM, and now IgE to support your research.
Learn more here
References
- Ding Z, Mulder J, and Robinson MJ. The origins and longevity of IgE responses as indicated by serological and cellular studies in mice and humans. Allergy. 2023 Dec;78(12):3103-3117. https://onlinelibrary.wiley.com/doi/10.1111/all.15799
| Learn more: | Do more: |
|---|---|
| Indirect and direct Western blotting | Exhibition Schedule |
| Chemiluminescence western blotting | Cite and Win |
| An Introduction to Expansion Microscopy | Past Competition Winners |



