

Congratulations to the recipient of Jackson ImmunoResearch’s €1000 travel grant for AACR 2019!
Jackson ImmunoResearch continues to offer travel funding to support researchers attending academic meetings and conferences.
JIR invited applications from attendees of the American Association of Cancer Research 2019 conference in Atlanta Georgia to receive a travel award of €1000 to be used against cost incurred attending the meeting.
AACR’s 2019 annual meeting aims to cover the latest discoveries across the breadth of cancer research—from population science and prevention; to cancer biology, translational, and clinical studies; to survivorship and advocacy. AACR offers a platform to highlight the work of the best minds in oncology research and medicine from institutions worldwide.
Find more information about the American Association of Cancer Research conferences here.
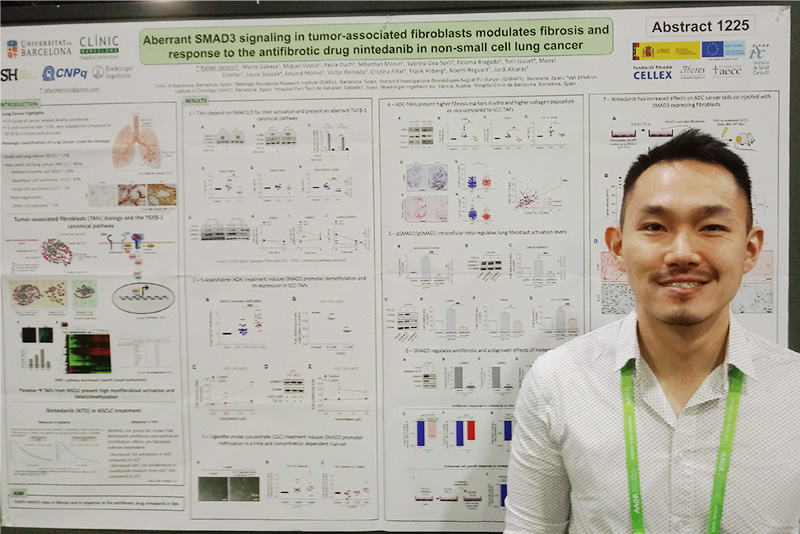
Travel award winner AACR 2019
The recipient of JIR’s AACR 2019 travel grant is Rafael Ikemori, a biologist currently working as a Post Doc at the University of Barcelona, Spain at the Unit of Biophysics and Bioengineering. Rafael has a PhD in Sciences in the field of oncology, for the last 3 years, he has been working as a postdoc in the lab of professor Jordi Alcaraz.
Read about his research and his experience at the AACR 2019.
“My main field of study is the tumor microenvironment in the non-small cell lung cancer. Particularly, I study the differences in the fibrotic behavior of tumor-associated fibroblasts derived from adenocarcinoma and squamous cell carcinoma patients. I analyze the differences in the TGFβ-1 canonical pathway in these cells and I have discovered significant differences due to smoking, which lead to decreased fibrotic markers especially in squamous cell carcinoma associated fibroblasts. I really enjoy my work because I also could link my data to differences in responses to drug treatment, making my research more translational.”
Attending AACR 2019
“I’ve been in the oncology field for more than a decade and I have always dreamed of attending the American Association of Cancer Research Symposium. Such incredible minds have passed by these meetings and many of them received a Nobel prize. I really enjoyed all my days here and they were quite busy with all the incredible presentations. Unfortunately, I couldn’t go to all of them, but luckily I can catch them with the webcast available on the internet. The work that I presented here is a huge project that started small but eventually will lead to significant discoveries that we will explore even more in future projects in my lab. I enjoyed a lot discussing my data with other scientists and I see that the tumor microenvironment field has grown a lot in the last years and I hope it will grow even more. And I’d like to thank my supervisor for giving me the opportunity to be here in this amazing meeting.”
Poster
Aberrant SMAD3 signaling in tumor-associated fibroblasts modulates fibrosis and response to the anti-fibrotic drug nintedanib in non-small cell lung cancer
Rafael Ikemori 1, Marta Gabasa 1, Miguel Vizoso 2, Paula Duch 1, Sebastian Moran 2, Sabrina Gea-Sorli 3, Paloma Bragado 3, Toni Jauset 4, Manel Esteller 2, Laura Soucek 4, Eduard Monsó 5, Víctor Peinado 3, Cristina Fillat 3, Frank Hilberg 6, Noemí Reguart 7, Jordi Alcaraz 1.
1Univ. of Barcelona, Barcelona, Spain; 2Bellvitge Biomedical Research Institute-IDIBELL, Barcelona, Spain; 3Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain; 4Vall d’Hebron Institute of Oncology (VHIO), Barcelona, Spain; 5Hospital Parc Taulí de Sabadell, Sabadell, Spain; 6Boehringer-Ingelheim Inc, Vienna, Austria; 7Hospital Clínic de Barcelona, Barcelona, Spain
A hallmark of non-small cell lung cancer (NSCLC) is a fibrotic/desmoplastic stroma rich in activated fibroblasts, which are critical regulators of cancer progression, response to therapies and radiotherapy resistance. Paradoxically, we recently reported that the important pro-fibrotic TGF-β transcription factor SMAD3 was epigenetically down-regulated through promoter hypermethylation in tumor-associated fibroblasts (TAFs) from NSCLC patients compared to patient-matched control fibroblasts. In addition, we reported that the clinically approved antifibrotic drug nintedanib elicited a stronger inhibition of both the fibrotic phenotype and its associated tumor-promoting effects in TAFs from adenocarcinoma (ADC) patients compared to squamous cell carcinoma (SCC) patients upon TGF-β1 stimulation in vitro, which was consistent with the selective therapeutic response to nintedanib observed in a clinical trial in ADC (but not SCC) patients. Altogether, these previous results suggest that TGF-β1 signaling may be altered in lung TAFs, and that such alteration may depend on their histologic subtype. In this study, we addressed these questions by determining the expression and activity of SMAD3 and its closely related homologue SMAD2 in patient-derived TAFs and paired control fibroblasts, and by dissecting their potential contribution to the differential therapeutic responses to nintedanib observed in ADC and SCC. In vitro studies revealed a marked SMAD3 epigenetic repression through promoter hypermethylation, a low pSMAD3/pSMAD2 ratio, and a limited fibrotic phenotype selectively in SCC-TAFs. In contrast, ADC-TAFs overexpressed a panel of fibrotic markers upon TGF-β1 stimulation concomitantly with a high pSMAD3/pSMAD2 ratio and limited SMAD3 promoter methylation.
Histologic analysis of a large patient cohort (112 ADC, 96 SCC) confirmed that the extent of fibrosis is larger in ADC than SCC patients. In addition, knocking-down SMAD3 in ADC-TAFs was sufficient to reduce the antifibrotic and antigrowth effects of nintedanib in vitro and in tumor xenografts in vivo. On the other hand, long-term exposure of pulmonary fibroblasts to cigarette smoke condensate was sufficient to hypermethylate the SMAD3 promoter. Since SCC and ADC tumors typically arise in the upper airways and distal pulmonary sites, respectively, it is conceivable that fibroblasts might be more exposed to the smoking epigenetic effects on SMAD3 in SCC. In summary, we report for the first time that tumor fibrosis is higher in ADC than SCC patients, in association with a selective therapeutic response to the antifibrotic drug nintedanib in the former, and identify the subtype-specific extent of SMAD3 epigenetic repression in TAFs and the subsequent aberrant SMAD3/SMAD2 imbalance as major regulatory mechanisms of tumor fibrosis and response to nintedanib in NSCLC.
There are still further opportunities to apply for JIR’s 2019 travel grants for selected conferences here!
| Learn more: | Do more: |
|---|---|
| Direct and indirect Western blotting | Exhibition schedule |
| Choosing your secondary antibody | NIR conjugates for Western Blotting |
| Colorimetric Western blotting | Cite and win! |


